Iliotibial Band Syndrome
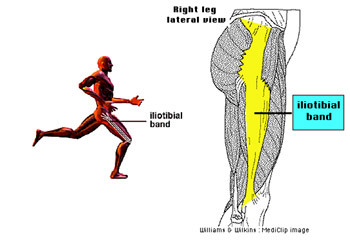
The Iliotibial band is a connective tissue band that runs down the lateral aspect (outside) of the thigh. It is a continuation of the tendinous partof the tensor fascia lata muscle and provides its attachment to bone.
In summary, the Iliotibial band runs down the outside of the leg between the top part of the hip and the upper tibia (shin bone).
Iliotibial band syndrome occurs due to friction between the iliotibial band and the underlying lateral femoral epicondyle, which is a bony prominence of the thigh bone at the knee joint. As the knee is bent and straightened repetitively the iliotibial band moves backwards and forwards over this bony prominence. Problems can occur with this mechanism and may lead to iliotibial band syndrome.
Symptoms:
- An ache over the outside of the knee usually after running for roughly the same time / distance on each run.
- Pain may disappear soon after running.
- Tenderness on the outside of the knee joint when palpated.
- Local inflammation is occasionally present around the outside of the knee.
- As the condition progresses there may be a sharp stinging pain, or burning on the outside of the knee.
Pain is likely to be aggravated by:
- Running over a certain distance / time.
- Running down hills.
- Running on cambered surfaces.
- Walking up / down stairs.
Common Causes:
- A significant / sudden increase in training intensity.
- Increased training on hills, uneven or cambered ground.
- Excessive foot pronation (turning inwards of the foot on impact).
- Incorrect or worn shoes.
- Tightness of the iliotibial band.
- Bow legs or knees which turn inwards.
- A leg length discrepancy.
- A lateral tilt of the pelvis.
Treatment:
- Reduce training load and intensity so running remains ‘pain free’.
- Apply ice to the knee (10mins approx every 2-3 hours). Wrap the ice pack in a damp cloth.
- Use non-steroidal anti-inflammatory drugs (eg. Ibuprofen) regularly for 5-7 days. Consult your pharmacist or General Practitioner for recommended dose.
- Massage therapy to decrease tightness of the iliotibial band. Get someone to use their forearm and apply pressure to the outside of the thigh starting at the knee and sliding slowly towards the hip. You can also try using a rolling pin to self-treat.
- Gentle stretching of the iliotibial band approx 3 times daily, holding stretches for 30 seconds.
Stretch 1:
In sitting, with your legs straight out in front, cross the affected leg over the other. Bend the affected leg at the knee so that the foot moves towards the opposite hip. Pull the affected knee towards the opposite shoulder using the opposite arm.
Stretch 2:
In standing, with both knees straight, cross the affected leg behind the other. Bend the upper body away from the affected leg whilst sticking out the hip on the affected side.
- Ensure appropriate footwear. You may require motion control shoes or orthotics to control over pronation. Gait analysis can be used to determine this.
- Avoid excessive downhill running or running on cambered surfaces.
- If running on a track alternate between running clockwise and anti-clockwise.
- On full recovery from iliotibial band syndrome decrease the risk of reoccurrence by the following preventative measures:
- Gradually increase training intensity.
- Continue iliotibial band stretches regularly.
- Ensure footwear remains correct.
- Ensure adequate strengthening of the gluteals, quadriceps, hamstrings and calfs within your training program.
- Avoid excessive downhill running or running on cambered surfaces.
- Ensure adequate rest within your training programme.
Similar Posts:
- Iliotibial Band Syndrome
- What You Need To Know About Iliotibial Band Injuries
- Runners Knee
- What Are Shin Splints?
- What is Plantar Fasciitis
- What Are Shin Splints And How To Avoid Them